Finance
What You Need to Know About HCC Risk Adjustment Coding
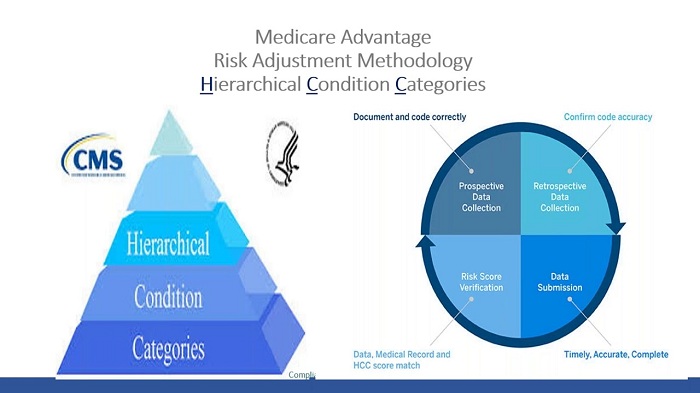
If you’re a healthcare professional, you’ve probably heard of HCC risk adjustment coding and may wonder how it works. HCC risk adjustment coding is a payment model that calculates a risk score based on a patient’s health status and demographic information to establish a baseline for how much it will cost to provide care to that patient.
Hierarchy Elimination of HCC Risk Adjustment Coding
Hierarchical condition category (HCC) risk adjustment coding is a critical component of Medicare’s value-based payment system. This model helps healthcare organizations estimate future Medicare Advantage costs and determine appropriate physician remuneration. As the value-based payment model gains traction, more healthcare organizations are beginning to incorporate it into their processes.
The HHS-HCC risk adjustment model incorporates the patient’s diagnoses and demographics to create a stable, clinically meaningful coding system. However, it is important to remember that ICD-9-CM codes must be grouped into logical categories to ensure they are properly coded and classified. In addition, diagnostic classification determines whether the risk adjustment model will discriminate between high-risk and low-risk patients. This consideration is vital for real-world risk adjustment.
The CMS-HCC risk adjustment model uses base-year diagnosis codes and demographics, while the HHS-HCC risk adjustment model uses current-year demographics and patient-specific diagnoses. Each person’s diagnosis and risk factors can affect current and future costs differently. The HCC risk adjustment models should reflect these differences.
Importance of Data
HCC risk adjustment coding is an important process for determining the relative risk for a patient. Although a health plan’s data on a patient does not directly affect his risk score, it is important to include the data for risk adjustment purposes. In addition, health plans can use this data to determine additional benefits for their members.
Accurate documentation of chronic conditions is essential for the risk adjustment process. For this purpose, providers must accurately document the conditions evaluated during each face-to-face visit. In addition, accurate documentation will impact treatment plans and ultimately result in accurate coding for HCC.
It is also essential for health plans to develop a regular cadence for monitoring coding quality. To do this, they must utilize all the tools available to ensure that their members receive accurate documentation. Accurate documentation of health conditions helps to ensure timely care.
Impact on Reimbursement
Achieving accurate HCC risk adjustment coding is critical to maximizing reimbursement. Healthcare organizations must meet strict guidelines to ensure the quality of HCC coding. They must document all patient encounters in the calendar year, and the documentation should support the diagnosis. In addition, the documentation must be precise. Generally, doctors document their care reasonably well, but they may be unaware of the details necessary to select the most appropriate code for each patient.
Inaccurate and inconsistent documentation puts payers and healthcare systems at risk. For example, suppose a clinician treats a patient for diabetes but does not enter an HCC code for diabetes. In that case, the payer will assume that the patient is healthier, thus resulting in lower reimbursement.
CMS is introducing changes to the HCC risk adjustment coding model to increase reimbursement accuracy. HCC coding has become essential to the financial success of medical groups and the effectiveness of value-based programs like Medicare Advantage.




![[pii_email_4c910535350b5a41ee81] Error Code Resolved](https://wigily.com/wp-content/uploads/2020/09/pii_email_4c910535350b5a41ee81-Error-Code-Resolved.jpg)